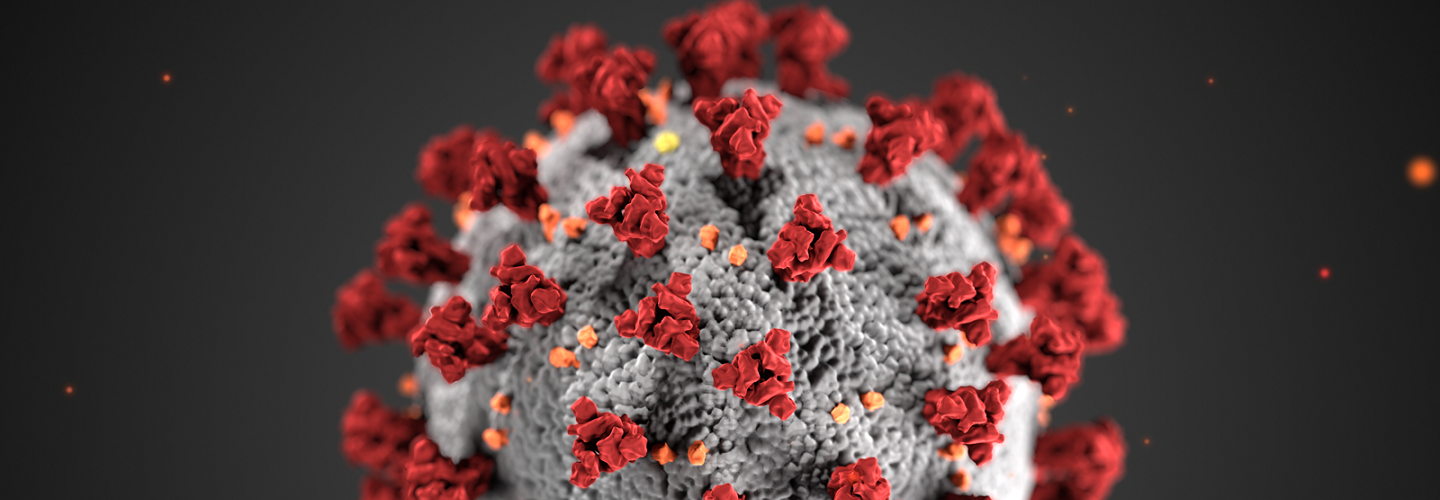
Academics suggest that the country’s initial responses to COVID-19 were adversely affected by the legacy of marketisation of its health system.
By Mr Shamim Quadir (Senior Communications Officer), Published (Updated )
Published in the journal, BMJ leader, a new commentary article suggests that China’s initial responses to the outbreak of the COVID-19 pandemic were affected by the legacy of changes made to marketise the country’s health system since shifting to a market economy in 1984.
Authored by academics from the Huazhong University of Science and Technology (Wuhan), the University of York, City, University of London and the Zhongnan University of Economics and Law (Wuhan), suggests that despite efforts to reform the health system since 2009, including a government commitment to transform the funding and organisation of primary care, it persists in being market-based.
The authors argue that this system encourages even public hospitals and community health centres to compete with each other. Maximising their own patient turnover to ensure their continued financial viability, and creating and maintaining perverse incentives, including the over prescription of medicines and the irrational use of services and technology. For example, price mark-ups on drugs still accounted for 30% of China’s public hospital income in 2018.
Crucially they say that marketisation has ensured that secondary care (acute and tertiary hospitals), and in particular the higher status tertiary hospitals, have been able to secure the lions share of funding at the expense of primary care (community health centres, and GP care).
This resource gap has allowed these hospitals to improve their staffing levels, facilities and service quality, while the community health centres, which are less able to compete in this market, have found it harder to recruit or invest in community-based and preventative services, further undermining public confidence in the quality of their services and ultimately demand.
Outbreak of COVID-19 and response
The commentary article suggests that the outbreak of the pandemic in Wuhan, Hubei province, highlighted how weak and fragmented China’s health system has become with a marketised model of care, which significantly hampered the country’s response.
For example, in the early days of the pandemic, people with the range of potential symptoms of COVID-19 descended en masse to hospitals in the region, rather than to community health services, which conversely reported comparatively low numbers of visits, given the reach of the disease.
The authors believe that patients taking this direct route to hospital, rather than to community health services, was a failed opportunity for community health services to act as an early warning system for the scope of disease transmission; led to hospital beds and services in the region being completely overwhelmed; and led to significant cross contamination of patients and health care workers with COVID-19 onsite at hospital.
For example, In Wuhan’s Zhongnan Hospital, between the 1st and 28th of January, 2020, it was estimated that 41% of cases were infected within the hospital, 29% of whom were healthcare workers.
However, the response of government to curb the initial surge of COVID-19 and bring the pandemic under control is well-documented and in line with the intentions of its 2009 health system reforms.
Whilst a key remedial action was the speedy construction from scratch of ‘Fangcang’ shelter hospitals to triage and treat patients with minor illnesses, other key actions were a formal gatekeeping and triage role of community health centres; the redeployment of clinical expertise, including GPs; and further resource from primary care to other parts of the health system.
Dr Yaru Chen, is a Research Fellow at the Centre for Healthcare Innovation Research (CHIR) at City, University of London and co-author of the study. Reflecting on the article she said:
Find out more
Read the commentary article in the BMJ Leader: 'Overcoming the legacy of marketisation: China’s response to COVID-19 and the fast-forward of healthcare reorganisation'.
Visit the Centre for Healthcare Innovation research webpage.